Jim Allison Won a Nobel Prize for His Cancer Breakthrough. But It Took Years for the Medical Community to Listen
Jim Allison is not quite what you’d picture when you think “world-renowned scientist.” He’s got the lab coat, sure. Not to mention the Nobel Prize he picked up in 2018 for his revolutionary work in the field of cancer treatment. But then he goes and does something you wouldn’t expect, like perform with fellow Texan Willie Nelson. (Allison plays blues harmonica and has known Nelson since the ’70s.) To paraphrase Mean Girls, he’s not a regular scientist; he’s a cool scientist. An iconoclast even.
That’s because, for the past few decades, Allison has been working on something even more unexpected: using the immune system to treat cancer — as opposed to the more traditional pillars of surgery, chemotherapy, and radiation. That meant he was met with a fair bit of skepticism and resistance from the medical community along that way. That is, until the results became too conclusive to ignore…
Like all good heroes, Allison has a compelling origin story, something that made his lifelong crusade against cancer personal — he lost his mother to the disease when he was only 11, then an uncle, then an older brother, and has been diagnosed three times himself. Then came the major breakthrough: following years of drug trials and painstaking research, Allison helped bring a cancer drug known as “ipi” or “Yervoy” to market in 2011, which has since helped save well over half a million lives. Hence why the Nobel committee came calling last year.
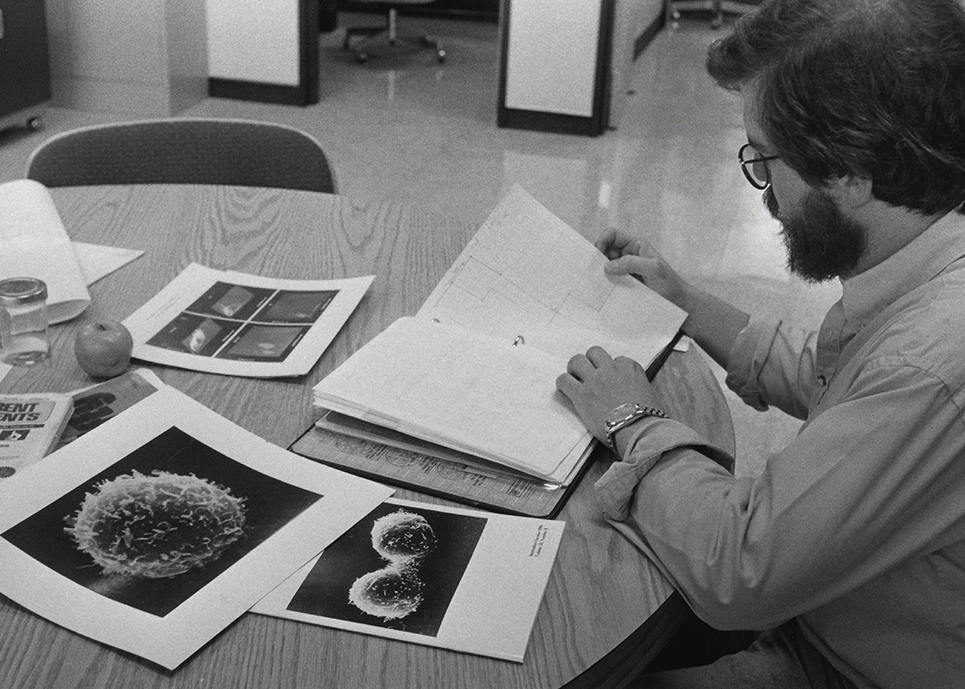
In theatres today, a documentary called Jim Allison: Breakthrough, from The Last Mountain director Bill Haney, follows Allison’s improbable journey, from his crucial discovery of the T-cell receptor in the early ’80s — considered “the Holy Grail of immunology research” — to receiving science’s ultimate honour in Stockholm. We spoke to Allison about how he kept pushing ahead in the face of skepticism, and the value in approaching a massive problem like “curing cancer” from an unconventional direction.
I have to tell you, when I found out I’d be interviewing a Nobel Prize-winning scientist, I wasn’t expecting the documentary to start out with a story about you getting your arm caught in a washing machine as a kid…
[Laughs.] That wasn’t the brightest thing I’ve ever done, no.
Then again, I wasn’t expecting it to end with you performing on stage with Willie Nelson either. You don’t seem like the stereotypical scientist.
Yeah, I guess. I don’t know. I’ve just always believed in doing what’s fun. Which I guess is a little different. I work hard, but I also try to play hard and have a good life.
Do you see Nelson as something of a kindred spirit? If he’s outlaw country, are you an outlaw scientist?
Yeah, I guess it’s not much of a stretch. I grew up with Willie’s music, in South Texas. His old songs, like “Hello Walls” and “Crazy” and all those classics. I was living in Austin in the ’70s when he moved there, when he made that big shift and got tired of people telling him what to do. So yes, I think I see some parallels there. I don’t want to say we grew up together, but we did, in some ways, follow parallel tracks over the last 50 years.
“Five years ago, the question was, ‘Does it work?’ The answer now is ‘Yes, absolutely. Now, how do we make it better?’ ”
So how did this documentary come about?
Well, I’ve been in the field long enough where I know quite a few people, not just in immunology, but in other sciences. There’s a very highly-respected molecular cancer biologist named Tyler Jacks that I’ve known for some time, from MIT. He approached me after a meeting a couple years ago and just said that he had this friend, an old roommate, bright guy, who makes documentaries and he had decided he wanted to make a film about me. And just don’t hang up. I get a lot of stuff, from people wanting to write this, write that, and you just ignore them. But Tyler said, “This guy Bill Haney’s going to call you.” And Bill called and I met him and he described to me what he wanted to do, and I thought, “Well, it’s a little scary, but yeah, OK.”
He had the best of intentions. Because he’d heard something about… I guess I had something of a reputation amongst people, scientists, for being a little unconventional. [Laughs.] But also the fights that I was having trying to get my ideas across — it attracted a fair amount of attention, and he felt he’d like to come along during the course of it and hopefully make a movie that would interest people in science. And, most importantly to me, to also show to young people that you can do science and still have fun. You don’t have to be the stereotypical pencil neck, sitting around in a lab all the time. So I said, “OK, I’m in.” Warts and all.
I know this movie is only an hour and a half, but in real time, this was a decades-long struggle for you to get to where you are now. Did you ever get frustrated? How do you keep going in the face of that?
First of all, if you’re going to be a scientist, you’ve got to be used to being frustrated. Because if you’re doing what at least I think you ought to be doing — and that’s looking into the unknown and trying to make some sense of it, trying to understand things that are not understood — you don’t know what the answer is when you start out.
One of the things I know about science is, the whole game’s not about just having an idea and doing experiments that’ll give you results that are consistent with what you think, but experiments that can only come out the way they do if you’re right. And that’s hard. But I felt that I’d done that. Up until the time I felt I’d done that, it was fair game. If somebody says, “Well, what about this?” Pointing out some other fact. That sort of stuff doesn’t bother me.
It was when all the data together was just, to me, completely irrefutable. That we had not only found this circuitry that downregulates immune responses, but that one could, in a predictable way, manipulate it to get the immune system to detect cancer. We did every experiment you could imagine in mice. And yet people said, “Oh, it’ll never work in humans.” The logic of that escapes me. I mean, just because it works in mice does not mean it’s going to work in humans, but to say you’re not ever going to try it in humans… That bothers me.
I also could not understand, nor could I accept, the idea that, oh, there might be some patents along the way, people got the biology wrong, but maybe they had [the patent]… Stuff like that, I did not deal with very well. That kind of stuff made me angry.
I can imagine.
So there were a few years of that, which took their toll. Because you can’t fight that kind of stuff. Logic doesn’t work, and data doesn’t work. That’s the only time it really got to me. I was in France, having a beer and I just said, “I don’t know what the hell I’m doing anymore. I’ve got something that’s not going anywhere and I don’t know what else I can do.”
Where were you met with more skepticism: the medical establishment or drug companies?
It was both. Drug companies are a hard place. They try 10 things, maybe 1 out of 10 work. So, if you work for a drug company, you’re not going to get fired for killing a program [early], you’re going to get fired for not killing one that cost the company a bunch of money. So it’s risky for people in drug companies. I grew to understand that. Luckily, I had some really courageous people working with me at Bristol Myers-Squibb willing to take that chance.
But there was a lot of skepticism amongst the scientists at the time, and I understand where they were coming from. The War on Cancer was announced by Nixon, so the prominent molecular biologists of the day said, OK, well, to fight cancer, we’ve got to understand cancer. And in order to understand that, we have to understand what controls normal growth. And just through the Human Genome Project, the spectacular advances that were made in biology really pretty quickly and efficiently allowed those cancer biologists, collectively, to understand what cancer is. It’s a genetic disease: we have mutations, and the normal regulatory things that regulate whether a cell divides or not, and whether it dies when it ought to or not, it moves somewhere else when it ought not to — these are the things that, when there’s a mutation, it kills the pathway that controls that, and makes the cell become a cancer cell.
So it makes a lot of sense then to try to identify those and come up with ways of blocking those enzymes. Of course, my approach was completely different. And while I respect that stuff, I felt, well, there are limitations there, and one of them is that there’s so many mutations that you’re not going to be able keep up. It’ll be Whac-A-Mole, one after the other. You can slow it down, but you can’t cure it.
And that’s where immunology comes in?
The immune system just attacks things that ought not to be in your body; wherever they come from and whatever they do, that doesn’t matter. If they’re not supposed be there, the immune system’s going to try to get rid of it. So, with that fundamental assumption, I thought maybe this is a better way to go. But there was a lot of skepticism.
The idea of getting the immune system to detect cancer is so compelling. Both philosophically and scientifically. Philosophically, it’s a comfortable thing; the idea that we could deal with [cancer] without having to do poison and burns and all that stuff. But people had been trying for a long time and nothing had ever worked. So there was a lot of failure. In my opinion, people published too fast, got in the headlines too fast, before they knew what they were doing. They just got over the tips of their skies a little bit. I felt it was important to understand the science intimately, and I felt I was in that position — I knew exactly the molecules we were talking about, what they did, and how to manipulate them. It wasn’t just like I was messing around with this. It was, “I know how this pathway works and I know how to get a desired outcome.” Those are two very different things. But people tarred me with the same brush… It was just a burden that I had to put up with.

I feel like this movie makes a pretty strong argument for the benefits of stepping back from conventional wisdom though. The value in thinking about a problem in a different way.
Absolutely. Ultimately, if I reduce this to trying to explain it in a bar somewhere… If somebody said, “Wait a minute, you’re not doing anything with the cancer cell.” No, we’re not. “Well, how can you treat cancer by ignoring the cancer cell?” Uh, because I think it’ll work? [Laughs.] We don’t need to mess with the cancer cell. We can get the immune system to do that. It’s almost a Zen-like approach to cancer therapy — which, in and of itself, created quite a bit of skepticism.
But I think it’s absolutely important, and that has been something that I try to do occasionally: just try to forget everything I’ve read, to the extent that I can, forget all the assumptions I’ve made, and try to reduce something just to the rawest elements and start building them back with what I know and what makes sense and see what I end up with.
This is something that’s brought up in the documentary, but obviously, this isn’t the end of this story. It’s really just the beginning. So what’s next for both you, and for this field in general?
Well, I think what we’re realizing now is that this does work, and with a certain fraction of patients with many different kinds of cancer, it can be curative — and I use that cautiously. But I think when somebody has had all their tumors disappear and hasn’t had any treatment for eight years or so, and the statistics show that they’re not going to need anymore, then maybe you can say they’re cured. But it’s still a fraction.
The best results are in combination with melanoma, where it’s approaching 60 per cent of people have multi-year survivals after therapy. Kidney, bladder, some other cancers are maybe 50 per cent or a little less. Dr. Pam Sharma [who Allison married in 2014] and I run a therapy platform here at the university [MD Anderson in Houston], and our whole goal is to look into patients that are receiving these drugs, or others that impact the immune system, and then dissect the tumor itself, molecularly, and see what’s going on. We know how to recognize a good response and figure out what’s missing and what we need to add next to get the perfect cocktail. Or a better cocktail, anyway.
And I’m convinced that by doing this, we’ll be able to have an impact on the majority of people, with many kinds of cancer. But I think it’s going to take combinations of multiple agents — not just immunological agents, but with chemo and radiation. Right now, people who do chemo or radiation try to kill that last cancer cell, because that’s the only way they’re going to be able to cure it. But now we know they don’t have to do that; all they have to do is kill enough to alert the immune system, and the immune system will take care of it. So we can take a pinch of chemo and radiation, and perhaps spare patients the bad consequences of that and give them the good.
I’m really optimistic that we’re going to grow from here over the next five to ten years and be able to treat many people with many different kinds of cancer. We’re not going to be able to cure all cancer, that’s not going to happen. Not now, not in the foreseeable future. But I think many of them, we will be able to treat. There’s a lot of work to be done… But five years ago, the question was, “Does it work?” The answer now is “Yes, absolutely. Now, how do we make it better?” So now at least the question’s easier, man.